Or…..we have to eat too!
I herewith recite some of the
teachings of my erstwhile teacher and career-long colleague, Mike Rie, now of
the University of
Kentucky and paraphrase an abstract we presented at ASA
in 2003 called:
“Pareto
Economics: Research Ethics And Law Violations In Interventional Continuous
Quality Improvement (CQI) Reports”
 Recent reports offer examples of efficiency driven non
therapeutic CQI projects in Anesthesia and Critical Care (1,2,3). These reports
describe innovations in process designed to conserve resources but with no
intent to improve the outcomes of the patients involved in the reports. I expect those health care providers involved in implementing these processes did
not conceptualize that they were involved in the involuntary taking of quality
from the involved patients…. kind of
like eminent domain when they take your house for the new highway (or shopping
center). This is actually a medical form of Pareto economics.
Recent reports offer examples of efficiency driven non
therapeutic CQI projects in Anesthesia and Critical Care (1,2,3). These reports
describe innovations in process designed to conserve resources but with no
intent to improve the outcomes of the patients involved in the reports. I expect those health care providers involved in implementing these processes did
not conceptualize that they were involved in the involuntary taking of quality
from the involved patients…. kind of
like eminent domain when they take your house for the new highway (or shopping
center). This is actually a medical form of Pareto economics.
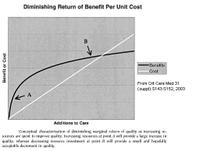
This conservation and
reallocation of resources assumes that the Pareto Improvements (4,5,6) in an
economic system depicted in the figure are both ethical and legal in health care
process innovation notwithstanding the constitutional protections when it comes
to eminent domain.
Pareto Economics. In an economic system a
Pareto improvement occurs if a person made better off can compensate a person
potentially worse off such that resources remain after such compensation. This
is used to lawfully justify public policy of building roads. If a property must
be taken by eminent domain to promote the public good, the American
Constitution provides that just compensation must be provided. As everyone knows this taking of property
certainly involves awareness of the “takee” with a due process recourse. Too bad the patients suffering involuntary taking of
quality are seldom aware and have little recourse for appeal or for
compensation. This leads to the notion
that not CQI but CQD is the process of our time… a time wherein health care
costs are predicted to double. That will
never happen. After all as a society,
we have to eat, provide for the common defense, and make sure our CEOs are well
fed.
Continuous Quality Decrement (CQD) Activities.
Industrial CQI methods have been widely incorporated into health care and
assume, for the overall good, that a small decrease of costly health care at
point B (figure) can be permissibly redistributed to point A. This application
of Pareto economics, usually implicit, underlies the managed care assertion
that enhancing preventive services safely permits and justifies decreased
budgetary allocations to expensive services like anesthesia and critical care.
This assumes that a small (even if difficult to measure) decrement in quality
at B is universally acceptable to those patients at B (or that they would
voluntarily accept economic recompense) so as to enhance preventive benefits to
patient populations situated at point A. However, this Pareto trade off in
health care has been ethically rejected in theory and by two prominent medical
consensus task forces (4,5,6). The a priori prediction that a small
diminution in quality to some patients at point B is acceptable represents an
untested population-based research hypothesis and imposition of an operational
moral value to patient care
Recent American
case law suggests that the Nuremberg Code of Ethics may now be legally
applicable, requiring changes in patient populations disclosure of
interventional CQI with accountability to IRBs (7,8,9) or perhaps others sorts
of ethical oversight. Given that these
patients who suffered involuntary CQD with no prospect of improved outcome and
clear risk of injury, one must wonder when this will be used as a legal theory
buttressing successful litigation that will change our style of treating
patients like widgets.
Conclusion. The creation of undisclosed Pareto
trade offs in health care clash with individual rights to previously agreed
upon contractual services in medical care and may constitute unethical and
illegal human experimentation. For maintenance of professional integrity and
public confidence in the medical profession, medical organizations should begin
public disclosure of the CQD decisions that are undertaken in our clinical
practices. In addition, editorial boards of peer-reviewed journals should
review their policies concerning ethical review of CQI/CQD type interventional
reports
References.
1. Anesthesiology 91:83947,1999
2. Anesth Analg 96:1104-8,2003
3. J Trauma 46:6259, 1999
4. J Health Econ16:131,1997
5. JAMA 276:11727,1996
6. Am J Respir Crit Care Med 165:54050,2002
7. Grimes v Kennedy Krieger Institute: Md Ct
of Appeals
366 MD.29, 782 A.2d 807;
8. Crit Care Med 31(suppl):S143-52,2003
9. Curr Opin Crit Care 3:329-33,1997
 Recent reports offer examples of efficiency driven non
therapeutic CQI projects in Anesthesia and Critical Care (1,2,3). These reports
describe innovations in process designed to conserve resources but with no
intent to improve the outcomes of the patients involved in the reports. I expect those health care providers involved in implementing these processes did
not conceptualize that they were involved in the involuntary taking of quality
from the involved patients…. kind of
like eminent domain when they take your house for the new highway (or shopping
center). This is actually a medical form of Pareto economics.
Recent reports offer examples of efficiency driven non
therapeutic CQI projects in Anesthesia and Critical Care (1,2,3). These reports
describe innovations in process designed to conserve resources but with no
intent to improve the outcomes of the patients involved in the reports. I expect those health care providers involved in implementing these processes did
not conceptualize that they were involved in the involuntary taking of quality
from the involved patients…. kind of
like eminent domain when they take your house for the new highway (or shopping
center). This is actually a medical form of Pareto economics.  Mitch Keamy is an anesthesiologist in Las Vegas Nevada
Mitch Keamy is an anesthesiologist in Las Vegas Nevada
 Andy Kofke is a Professor of Neuro-anesthesiology and Critical Care at the University of Pennslvania
Andy Kofke is a Professor of Neuro-anesthesiology and Critical Care at the University of Pennslvania
 Mike O'Connor is Professor of Anesthesiology and Critical Care at the University of Chicago
Mike O'Connor is Professor of Anesthesiology and Critical Care at the University of Chicago
 Rob Dean is a cardiac anesthesiologist in Grand Rapids Michigan, with extensive experience in O.R. administration.
Rob Dean is a cardiac anesthesiologist in Grand Rapids Michigan, with extensive experience in O.R. administration.

