Every now and then
you hear talks that astonish and fundamentally change the way you view some
issue or disease state. I heard one of these at this year’s Society for Neurosurgical Anesthesia and Critical Care (http://www.snacc.org/)
meeting in San Francisco in October 2007. This one was about the persistent vegetative state (PVS) and how not
all may be as it seems.
 Dr Adrian M Owen of the
University of Cambridge in the United Kingdom
presented his studies of functional Magnetic Resonanace Imaging (fMRI) in patients in the persistent
vegetative state (PVS) showing clear
evidence of awareness and cognitive ability in some of these patients.( fMRI uses the MRI to indicate areas of the brain that are active) His work has been formally published in
Science 313:1402, 2006.
Dr Adrian M Owen of the
University of Cambridge in the United Kingdom
presented his studies of functional Magnetic Resonanace Imaging (fMRI) in patients in the persistent
vegetative state (PVS) showing clear
evidence of awareness and cognitive ability in some of these patients.( fMRI uses the MRI to indicate areas of the brain that are active) His work has been formally published in
Science 313:1402, 2006.
PVS is a syndrome wherein a patient by every bedside test
shows no interaction with his/her environment. The patient does not attend to any external stimuli, does not track with
his/her eyes and seems totally unconscious. Families (like the Schiavo clan) however may be struck by the patient’s
apparent wakefulness, lack of need for a ventilator, and persistence of
ordinary vegetative bodily functions. The patient can look seductively awake but is not. Of this I was certain till I heard this talk.
Dr Owen presented the fMRI method whereby various inputs to
a subject in an MRI scanner can create reproducible patterns. For example tell a patient to think about
something and you get a stereotypical fMRI pattern. Tell a patient to think about riding a bike
or think about a specific place and different reproducible patterns of
activation arise in the brain. OK… neat.
Well Dr Owen presented a patient with all the stigmata of
PVS from traumatic brain injury with diffuse axonal injury. This vegetative patient, however, when asked
to think about a place or to think about riding a bike showed fMRI activation
absolutely the same as that produced when an ordinary awake patient responded
to the same command. In fact this
patient was fully able to interact with the investigators in this manner. “If you can hear me think about riding a
bike” leading to the bike riding
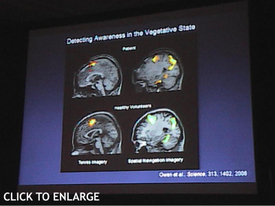
pattern. I took a picture of this slide
showing this and reproduce it here:
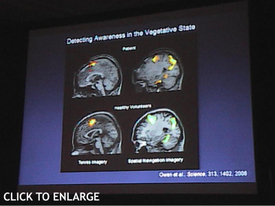 The fMRI of the PVS patient is at the top and the control
volunteers at the bottom. The left
images are
those of tennis playing imagery and on the right of spatial
recollection imagery. I believe this is going to have implications for decisions
about extent of life support in such patients. Certainly many(probably most) PVS patients really are in PVS. Unlike this
case, I don’t expect patients with neocortical death will be responsive like this. Nonetheless it does suggest that before we
make such PVS declarations that we should make sure on tests like those
presented by Dr Owen that the PVS patient really is in PVS.
The fMRI of the PVS patient is at the top and the control
volunteers at the bottom. The left
images are
those of tennis playing imagery and on the right of spatial
recollection imagery. I believe this is going to have implications for decisions
about extent of life support in such patients. Certainly many(probably most) PVS patients really are in PVS. Unlike this
case, I don’t expect patients with neocortical death will be responsive like this. Nonetheless it does suggest that before we
make such PVS declarations that we should make sure on tests like those
presented by Dr Owen that the PVS patient really is in PVS.
For starts, in those patients in whom we find that PVS is really “pseudoPVS,” I expect this will be an objective measure to use for rehab. Just keep thinking about that bike riding and
after awhile the physiatrists, wonder workers that they are, may be able to have
the patient really bike riding or doing other cognitive things. It will tell them to not give up.
So it seems that what we thought we knew for sure we’re not
so sure of anymore. Déjà vu.
 Dr Adrian M Owen of the
Dr Adrian M Owen of the
 Mitch Keamy is an anesthesiologist in Las Vegas Nevada
Mitch Keamy is an anesthesiologist in Las Vegas Nevada
 Andy Kofke is a Professor of Neuro-anesthesiology and Critical Care at the University of Pennslvania
Andy Kofke is a Professor of Neuro-anesthesiology and Critical Care at the University of Pennslvania
 Mike O'Connor is Professor of Anesthesiology and Critical Care at the University of Chicago
Mike O'Connor is Professor of Anesthesiology and Critical Care at the University of Chicago
 Rob Dean is a cardiac anesthesiologist in Grand Rapids Michigan, with extensive experience in O.R. administration.
Rob Dean is a cardiac anesthesiologist in Grand Rapids Michigan, with extensive experience in O.R. administration.