We have our medical students in the neuroICU make informal 15-30 minute summaries of issues relevant to our patients. We had a patient in our unit who had complex back surgery but had an indwelling drug eluting coronary stent that had been in place for several years. This is the summary provided which I reproduce here with permission of the student:
Perioperative Stent Management
Carter Clement, UPenn Medical Student April 23, 2024
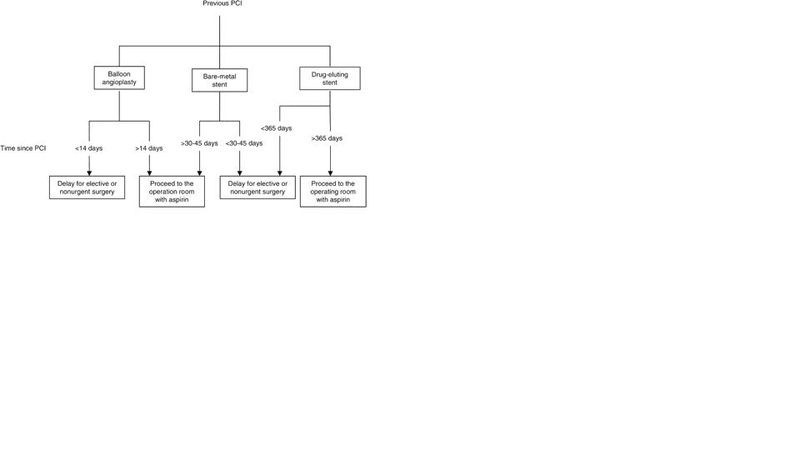
ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery (Fleisher et al)
1) Balloon Angioplasty
-Healing takes ~2 wks & surgery has high risk of thrombosis in this period
-Increased risk of restenosis after ~8 wks
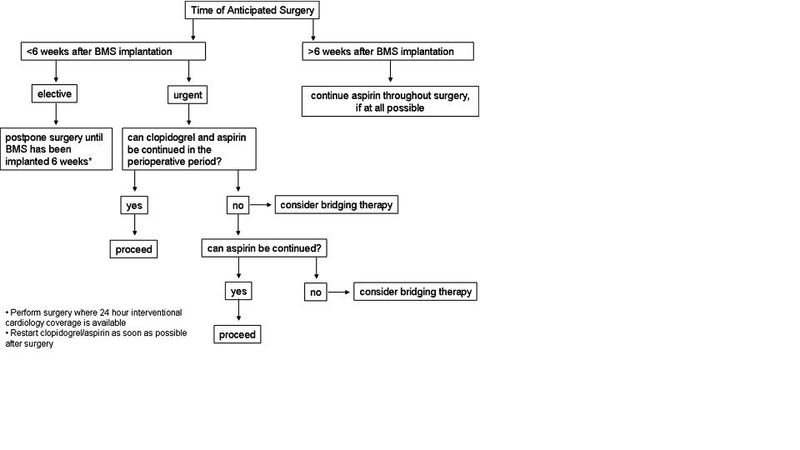
2) Bare Metal Stent (BMS)
-Endothelialization takes 4-6 wks & greatly reduces risk of thrombosis
-Dual antiplatelet therapy (DAT, ASA + thienopyridine) should be given during this period (usually x 4 wks)
-ASA alone should be continued beyond this period
-Thienopyridine effects persist ~1 wk after drug is stopped, so surgical risk persists in that time
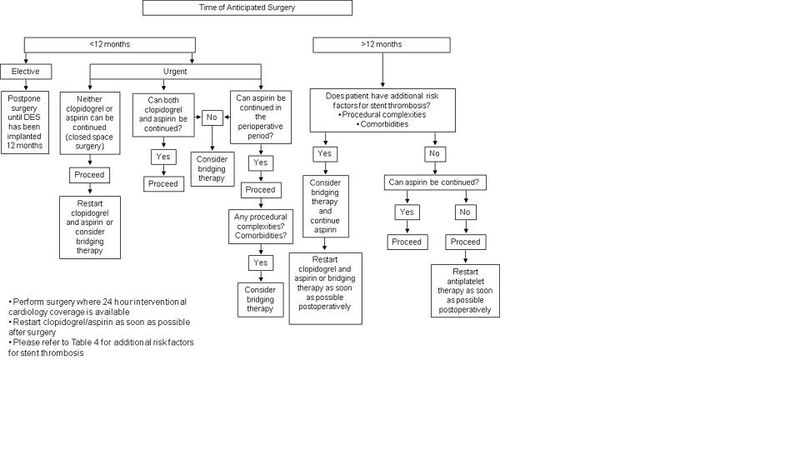
3) Drug Eluting Stent (DES)
-Well established risk of late thrombosis (up to 18 months) because drug elution prevents endothelilization
-DAT x 12 months, then ASA only
Other Perioperative Considerations:
-Generally, consider continuation of DAT beyond recommended time frames if high cardiac risk
-Consider continuation of DAT during surgery when possible, especially if:
-High cardiac risk & low bleeding risk
-Urgent surgery is necessary before the recommended non-surgical period has expired
(Exceptions: high risk surgeries such as neurosurgery - weigh risks and benefits on patient-to-patient basis)
 Mitch Keamy is an anesthesiologist in Las Vegas Nevada
Mitch Keamy is an anesthesiologist in Las Vegas Nevada
 Andy Kofke is a Professor of Neuro-anesthesiology and Critical Care at the University of Pennslvania
Andy Kofke is a Professor of Neuro-anesthesiology and Critical Care at the University of Pennslvania
 Mike O'Connor is Professor of Anesthesiology and Critical Care at the University of Chicago
Mike O'Connor is Professor of Anesthesiology and Critical Care at the University of Chicago
 Rob Dean is a cardiac anesthesiologist in Grand Rapids Michigan, with extensive experience in O.R. administration.
Rob Dean is a cardiac anesthesiologist in Grand Rapids Michigan, with extensive experience in O.R. administration.
Comments